Understanding Traumatic Brain Injury (TBI)
A Traumatic Brain Injury (TBI) is an injury that affects how the brain works. It can be caused by a sudden trauma, such as a bump, blow, or jolt to the head, neck, or body. It is not required that someone hit their head to suffer a TBI. For example, someone may be rear-ended in a car, and while their head is not hit, the quick movement of the head moving backward and forwards can be a sufficient jolt to their brain to result in a traumatic brain injury.
There are three main types of TBI: (1) a mild TBI, also called a concussion; (2) a moderate TBI; and (3) a severe TBI.
The symptoms of a TBI are variable in duration, intensity, and type. Some individuals have minor symptoms, such as headaches and tiredness, for a brief time, while others may have more significant symptoms, including prolonged memory loss or permanent physical and mental disabilities. Each TBI is different, and there is no one-size-fits-all approach to how they recover, the treatment that is needed, or the duration of symptoms.
Incidence, Prevalence, and Impact
Incidence is a measure of the number of new cases of a disease or condition that develop in a population over a given time period.
- In 2019, approximately 223,135 TBI-related hospitalizations occurred in the U.S.
- In 2020, there were 64,362 TBI-related deaths in the U.S.
- Approximately 23,500 emergency room visits each year are due to a TBI in Colorado.
- Almost 5,000 individuals are hospitalized and nearly 1,000 die due to a TBI in Colorado each year.
Prevalence is the proportion of the population who have a specific disease or condition in a given time period, regardless of when they first developed the characteristic.
- In 2010, an estimated 1.6 million Coloradans were living with a lifetime history of TBI and its effects.
- 57% of people who survive a moderate to severe TBI are moderately or severely disabled five years after injury.
Additional statistics and facts.
- Individuals aged 75 and older have the highest rates of TBI-related hospitalizations and deaths.
- Males are nearly twice as likely to be hospitalized and three times more likely to die from a TBI compared to females.
- High-risk age groups include children (0-17 years) and older adults (65+).
- Brain injury is the leading cause of disability and death in children and adolescents in the U.S.
- Colorado ranks 9th nationally in TBI-related fatalities and 13th in hospitalizations.
Risk Factors
Certain populations are more susceptible to TBIs, including:
- Females, elderly, sports injuries
- Military service members and veterans
- The Homeless
- Individuals in correctional and detention facilities
- People in abusive relationships
- Rural residents
Since 2000, nearly 400,000 military personnel have sustained a TBI.
Causes of TBI
The primary causes of TBI include:
- Falls
- Motor vehicle crashes
- Being struck by or against objects
- Assaults
- Other or unknown causes
Economic Impact
In 2000, the estimated direct and indirect costs of TBI were $60 billion in the U.S. Long-term consequences of TBI can include functional changes in thinking, language, learning, emotions, behavior, and sensation, as well as an increased risk of neurodegenerative diseases.
Common Questions
- What is a traumatic brain injury (TBI)? A TBI occurs when a sudden trauma causes damage to the brain. This can result from a blow, bump, or jolt to the head or a penetrating injury. It can also result when the head moves rapidly, such as in a rear-end collision or a fall. There is no requirement that the head actually be hit in order to sustain a TBI.
- What are the common causes of TBIs? Common causes include falls, motor vehicle accidents, sports injuries, and assaults.
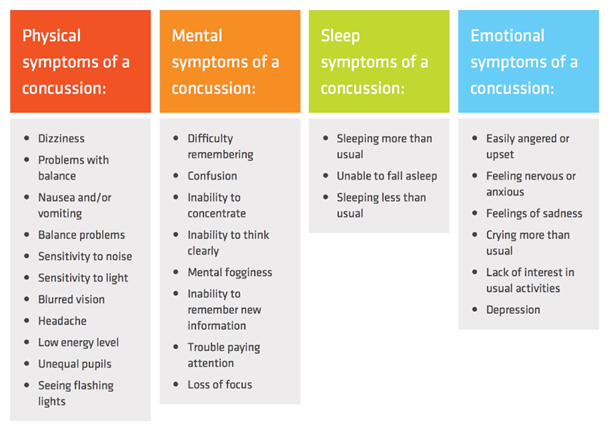
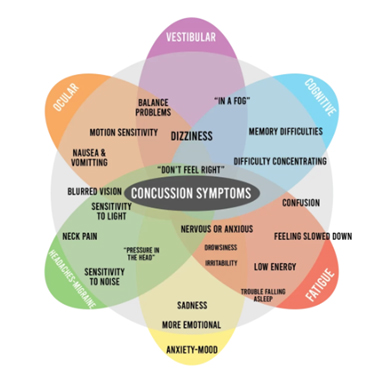
- What are the symptoms of a mild TBI or concussion? There is a large range of TBI and concussion symptoms that can vary in severity and duration. Symptoms can affect a person physically, mentally, emotionally, and cause issues with their sleep and vestibular/vision systems. Below are two reference charts providing examples of symptoms of traumatic brain injuries and concussions:
- How is a TBI diagnosed? A traumatic brain injury is diagnosed by a medical professional using one or more of the following: medical examination that evaluates an individual’s thinking, motor function, sensory function coordination, eye movement, reflexes, and other neurological considerations; the individual’s clinical presentation and symptom reporting; objective testing for balance, vision, and vestibular dysfunction; imaging tests like CT scans or MRIs; and neuropsychological or cognitive assessments. Mild traumatic brain injuries do not typically appear on a CT scan. For moderate to severe traumatic brain injuries, the medical practitioner may also use the person’s Glasgow coma scale (i.e., GCS is a tool that measures your ability to open your eyes, speak, and move to help determine the severity of the TBI) and blood tests.
- What treatments are available for TBI? Treatment depends on the severity and can include rest, medication, surgery, rehabilitation therapies, and ongoing medical care. It is important that someone with a TBI be assessed by a medical provider knowledgeable in traumatic brain injuries to ensure that they are obtaining the treatment they need to have maximum recovery.
- What is the difference between a concussion and a TBI? A concussion is another term for mild traumatic brain injury.
- How can TBIs be prevented? There is no way to prevent a TBI, however, there are strategies that will reduce the risk of suffering a TBI or that can reduce the severity of the TBI. Such strategies include wearing helmets, using seat belts, fall-proofing homes, avoiding drugs and alcohol, and following safety guidelines in sports and workplaces.
- What are the long-term effects of a TBI? There can be many long-term effects from a TBI, particularly depending on the severity. Such effects include but are not limited to, permanent symptomology (see above charts for symptom examples), cognitive impairments (including difficulty thinking clearly, understanding, learning, concentrating, or remembering information), motor and sensory issues (including weakness in extremities, difficulty with coordination and balance, and vision or vestibular problems), emotional and behavioral changes (including irritability, emotional, anxiety and depression, change in personality, aggression), neurological complications (including seizures, weakness, sensory deficits, and difficulty swallowing), physical disabilities, and increased risk of neurological diseases.
- How can family members support a loved one with a TBI? Support can include helping with medical care, providing emotional support, assisting with daily activities, being patient and understanding, and seeking professional guidance. Also, joining support groups for caregivers to assist with other ways to support their loved one or to assist in managing their own stress and feelings about the loved one’s injuries.
- 10. Where can I find resources and support for TBI? Resources are available through organizations like the Brain Injury Association of America, local support groups, and specialized healthcare providers. Click here for a list of resources.
